Genetic Testing and Tamoxifen: What You Need to Know
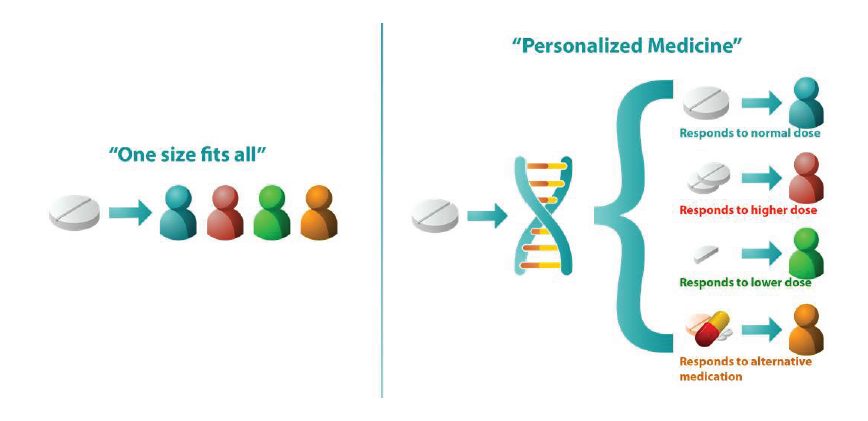
Have you been prescribed Tamoxifen? Did you know that genetic testing can identify how your body processes the medication. Are you getting the full benefit from the Tamoxifen or is your DNA leaving you at a higher risk of your cancer recurring?